Category: Electric Transfer Chair
Posted by 2025-12-29 11:12
hoyer lift guidelines medicare
Hoyer Lift Guidelines and Medicare Coverage: Key Information You Need to Know
For patients who cannot independently complete daily transfers due to illness, aging, or disability, a Hoyer Lift is not just an assistive tool, but a crucial device that ensures safety, dignity, and the sustainability of care. However, such equipment comes with a high price tag, and many families naturally wonder: Can Medicare help when considering a purchase?
The answer is: Under specific conditions, Medicare can indeed cover part or all of the costs of a Hoyer Lift. But to successfully obtain reimbursement, hoyer lift guidelines medicare you must strictly meet its criteria for medical necessity, prescription requirements, and usage standards. This article will clearly outline Medicare’s coverage policy for Hoyer Lifts and, combined with safe usage guidelines, help patients and caregivers make informed, compliant decisions.
How Does Medicare View Hoyer Lifts?
In the United States, Medicare classifies Hoyer Lifts as "Durable Medical Equipment (DME)." This means that as long as the equipment is used to treat or manage a medical condition and meets a series of strict standards, it may be eligible for reimbursement under Part B (Outpatient Insurance).
It is important to note, however: Medicare does not cover costs for "convenience" or "comfort." The equipment must be proven to be a reasonable and necessary medical intervention. In other words, you need to demonstrate that without this device, the patient would face risks such as falls, skin injuries, failed care, or even hospitalization.
Core Conditions for Obtaining Medicare Reimbursement
To have Medicare cover a Hoyer Lift, the following key requirements must all be met simultaneously.
First, a written prescription from a qualified healthcare professional is mandatory. This is typically a doctor, nurse practitioner, or physician assistant. The prescription cannot simply state "Hoyer Lift"; instead, it must detail the patient’s diagnosis (e.g., post-stroke hemiplegia, advanced multiple sclerosis, severe arthritis), functional limitations (such as being completely unable to sit steadily, bear weight, or cooperate with transfers), and why lower-level assistive devices (e.g., transfer belts, sliding boards) are insufficient to meet the patient’s needs.
Second, medical necessity must be proven. Medicare tends to approve coverage for patients who are fully dependent on others for transfers, weigh over 100 pounds (approximately 45 kilograms), have a high risk of falling, or already have pressure ulcers. If the patient can still partially stand or walk with support, Medicare may determine that a Hoyer Lift is not necessary and recommend trying more basic assistive methods first.
Third, the equipment must be primarily used in a home setting. If you or your family member lives in a long-term care facility recognized by Medicare (e.g., a skilled nursing facility), the costs of related equipment are usually borne by the facility and not covered under Medicare Part B.
Finally, the equipment must be obtained through a Medicare-certified DME supplier. These suppliers are registered with Medicare and agree to accept the payment amount approved by Medicare (i.e., "accept Assignment"), so they will not charge the patient additional fees. You can search for local certified suppliers on the official Medicare website (Medicare.gov).
Reimbursement Method: Rental or Purchase?
Medicare generally prefers to cover the rental of high-cost electric Hoyer Lifts rather than one-time purchases. hoyer lift guidelines medicare For manual hydraulic models, direct purchase reimbursement is sometimes available. Under the rental model, Medicare pays the monthly rental fee, and after 13 months of rental, the equipment typically becomes the property of the patient.
In terms of cost-sharing, the patient must first meet the annual Part B deductible (which is $257 in 2025). After that, Medicare covers 80% of the approved cost, and the patient is responsible for the remaining 20%. If you have a Medigap (Supplemental Insurance) policy or certain Medicare Advantage plans, this out-of-pocket amount may be further reduced or even waived.
Safe Usage: Not Just a Responsibility, but a Compliance Requirement
Even with Medicare reimbursement, using a Hoyer Lift correctly and safely remains the core of care. While Medicare does not mandate training, it strongly recommends that caregivers master basic operating standards to avoid accidents and ensure the equipment achieves its intended therapeutic effect.
The primary principle is to match the appropriate sling. Full-body slings, toileting slings, and floor rescue slings each have specific uses and must not be used interchangeably. The size of the sling must also match the user’s height and weight—an overly large sling may slip, while an overly small one can cause discomfort due to pressure. Before each use, always check the sling for wear, loose threads, or odors; aging slings should be replaced promptly.
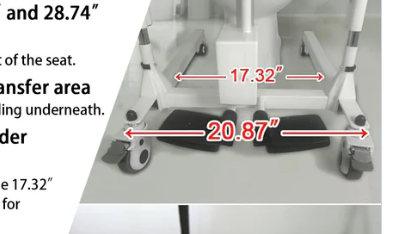
During operation, the lift’s legs should always be fully extended and locked to ensure the base is stable; lifting and lowering movements should be slow and smooth, avoiding sudden stops or oblique pulling; when transferring in narrow spaces (e.g., bathrooms), obstacles must be cleared in advance to prevent collisions.
It is particularly important to note that floor transfers have special requirements for equipment. hoyer lift guidelines medicare Standard Hoyer Lifts usually cannot get close to the floor, so a low-base or detachable-leg model must be used, paired with a dedicated floor sling. Forcibly dragging a user with ordinary equipment not only violates safety guidelines but may also be considered "improper use," which could affect future eligibility for DME reimbursement.
Application Process and Common Challenges
The process for applying for Medicare reimbursement for a Hoyer Lift typically involves the following steps: first, communicate your needs with a doctor and obtain a detailed prescription; then, contact a Medicare-certified DME supplier; the supplier will assist in collecting medical records and submitting the application to Medicare. In some states, complex DME requires prior authorization, and approval may take several days to several weeks.
Common reasons for claim denials include: incomplete prescription information, insufficient proof of medical necessity, use of a non-certified supplier, or the patient being deemed capable of using a lower-level assistive device. If your application is denied, you have the right to submit a redetermination request, along with supporting evidence such as a physical therapist’s assessment report, fall records, or other relevant documentation.
Conclusion: Policy as a Shield, Standards as a Sword
Medicare’s coverage of Hoyer Lifts reflects the public healthcare system’s respect for the basic living rights of people with disabilities. But policy is just the starting point—true care quality stems from attention to details, from a detailed doctor’s prescription to every smooth lifting and lowering operation.
By making good use of Medicare resources while strictly following safe usage guidelines, hoyer lift guidelines medicare this device can truly become a reliable partner in safeguarding the dignity of life. In an era of deepening population aging, understanding and applying these policies and standards is the most practical and gentle commitment you can make to your loved ones.